Eye Conditions
Eye conditions, such as cataracts, glaucoma or a detached retina are common in New Zealand. These conditions can eventually lead to blindness. Some eye conditions may relate to a problem in the brain. Others are related to issues within the eye itself. You can find out more about the most common eye conditions in New Zealand below.
There are many different eye conditions that thousands of New Zealanders face. Below you’ll find information about each of these conditions.
Cataracts
Cataracts refer to a cloudiness or marks on the lens inside the eye. Some babies may be born with cataracts, or they may develop in younger people due to other disease or damage to the eye. However, the majority of cataracts are associated with getting older. People with early cataracts may find that they have trouble driving at night, or need extra light to see fine detail. As cataracts develop, they can cause serious loss of vision, however in New Zealand, we have very effective surgical treatments available. The surgery involves using tiny instruments to remove the cloudy lens material, and a small artificial lens is inserted into the eye. Many people will need reading glasses to fine tune their vision following the surgery.
Cataracts are very common, and some people will have other eye diseases in addition to cataracts. Timing of cataract surgery will be tailored to the individual patient’s specific circumstances. Sometimes the surgeon will advise that removing a cataract will not be expected to improve vision, e.g. because of macular disease, and surgery is therefore not recommended. On the other hand, if a patient has diabetes, cataract surgery may be recommended early so that the eye specialists can preserve a good view of the retina, and make sure they spot any diabetic eye disease early.
Glaucoma
Glaucoma refers to a group of eye diseases where there is damage to the tiny fibres in the optic nerve. The optic nerve takes messages about what we see from the eye to the brain. About 2% of Kiwis over the age of 40, and about 10 % of those over 70 years have glaucoma.
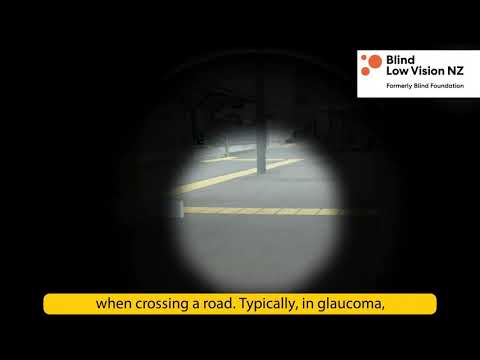
Some types of glaucoma have rapid onset with pain and sudden loss of vision. However, most people with early glaucoma notice no discomfort or change in vision. This is because damage to the nerve fibres occurs slowly over many years, and often peripheral vision is damaged first. Our brains are very good at filling in missing patches and combining the pictures from the two eyes. This means a person may not notice vision loss until the disease is advanced, with just a central area of tunnel vision remaining.
The good news about glaucoma is that for many cases, early detection leads to effective treatments, often with daily eye drops, or possibly laser or surgical treatments.
NZ guidelines recommend a glaucoma check up with your optometrist or ophthalmologist at age 45, and, if there are no symptoms or risk factors, the glaucoma eye check should be repeated every five years.
If vision has been lost due to glaucoma, that vison cannot be regained. Often people will have patches of vision missing above, and/or below the horizontal mid line. Central vision can also be damaged in later disease. People with glaucoma often notice that they have poor contrast sensitivity, this means that while they may be able to see black letters on a white background, they cannot pick out an item on a cluttered bench, or safely identify steps and kerbs.
Blind Low Vision NZ can help people to understand which part of their vision is not working well. This is especially helpful when they want to explain to family and friends what is going on. The specialists at Blind Low Vision NZ can help people to come to terms with their vision loss, and to learn to use new techniques or equipment to make the most of their remaining vision, so that they can continue to do the things that are important to them.
For more information, visit the Glaucoma NZ website.
Macular Degeneration
Macular Degeneration (MD) is the most common cause of vision loss in older people in New Zealand. Some rare forms affect children and younger people, but the vast majority of people with MD are in the older age groups. One in seven people over 50 will experience MD. We now know that many people have a genetic pre-disposition to developing Age-related MD (AMD). Smoking puts people at a higher risk of AMD; we know that eating a healthy diet and exercise are protective, but the number of birthdays is the greatest risk factor… not something we can control!
The macular is part of the retina. If you think of your eye like a camera, the retina is like the film in a camera. When a person has macular disease, it is as though there is a scratch or graze on film. This means even if the person has the correct glasses, the picture will still be distorted, or have patches missing.
Macular disease affects the central vision, this means that when the person looks straight at a face, at some reading material, or their watch, a distorted or blurry patch will stop them seeing clearly.
Most people with macular degeneration have the “dry” kind, which comes on and progresses very slowly. There is generally no treatment for dry AMD, but sometimes the specialist recommends dietary supplements to try to halt the degeneration.
Sometimes dry AMD changes to become “wet” AMD. We do have effective treatments for wet macular disease in New Zealand. Treatment usually involves injections into the affected eye. This sounds alarming, but many elderly New Zealanders have regular injections at the eye clinic, they generally cope very well with the procedures, which help them to retain the vision they have.
The success of treatment for wet AMD depends on beginning treatment early, as soon as the wet disease develops. If a person notices sudden changes in their central vision, or straight lines appear distorted, with a wobble or kink, then they should arrange to see their optometrist as soon as possible, ideally within a few days. The optometrist will be able to examine the retina and macula and refer on to an ophthalmologist if treatment is necessary.
The good news about AMD is that the disease is limited to the central vision. This is troublesome because it makes reading and recognising faces difficult, however the peripheral vision is not affected. People with AMD are able to move around without bumping into doorways and they can be reassured that they will never go completely blind.
Blind Low Vision NZ can help people to understand which part of their vision is not working well. This is especially helpful when they want to explain to family and friends what is going on. Staff at Blind Low Vision NZ can help people to come to terms with their vision loss, and to learn to use new techniques or equipment to make the most of their remaining vision, so that they can continue to do the things that are important to them.
To learn more, take a look at our Age Related Macular Degeneration Guide or visit the Macular Degeneration website.
Retinitis Pigmentosa
Retinitis Pigmentosa is often simply called RP. It describes several different hereditary diseases. With RP, vision loss is caused by the breakdown and loss of cells in the retina called rods and cones.
RP commonly runs in families and is a genetic condition. The age when someone first notices vision difficulties and the rate at which the vision deteriorates can vary widely – even within the same family. Most people will first notice something wrong between 10 and 30 years old.
People with RP first notice difficulty seeing at night, when there’s low light or going between light and dark places. Next they will find their peripheral (or outer) vision beginning to disappear. In some cases, the central vision is also affected.
RP is sometimes part of a syndrome, for example Usher Syndrome, when hearing and often balance are also affected.
There are many types of RP and associated rare retinal conditions. In order for someone to understand their individual condition, genetic testing may be recommended. This can provide information about what is most likely to happen in future, and whether emerging treatments may be helpful.
You can find out more about RP at Retina New Zealand and their international organisation Retina International.
Diabetic Retinopathy
Diabetic retinopathy is the condition caused by damage to your retina through diabetes. In diabetes, damage to the blood vessels in the retina can cause problems. The blood vessels leak or clog up and don’t let enough blood through – this can lead to vision loss.
People with diabetes are also more at risk of developing Cataracts and Glaucoma.
Although these are potential issues for diabetics, having diabetes does not necessarily lead to sight loss. If caught early, diabetic eye disease is usually treatable, with drug, laser or surgical interventions. Its progress can also be slowed through your own interventions – such as managing your diet and blood pressure.
If not identified and treated, it can however lead to significant vision loss and even blindness.
In New Zealand, all people with diabetes should have regular screening to check for eye trouble. Diabetes New Zealand recommends a full diabetes eye check when you first know you have diabetes. From that time on you should have a full eye check at least every two years. It is important that your doctor refers you to your local Diabetes Services Retinal Screening Programme, run by Diabetes New Zealand.
For more information about diabetic eye disease, visit the Save Sight Society website and select the ‘Diabetes’ tab.
Other eye conditions include:
- Albinism is a condition where people have little or no melanin pigment in their eyes, skin or hair. As development of the optical system is dependent on melanin, it means that people with albinism can have low vision. You can find out more at New Zealand’s Albinism Trust)
- Charles Bonnet Syndrome causes a person whose vision has started to deteriorate to see things that aren’t real (hallucinations). The hallucinations may be simple patterns, or detailed images of events, people or places. They’re only visual and don’t involve hearing things or any other sensations.
- Cortical Visual Impairment is used to describe a visual impairment that occurs due to brain injury. Rather than being a physical problem with the eye, it is caused by damage to the brain. It means the eyes can see but the brain is not interpreting what is being seen.
- Keratoconus is a degenerative condition which causes the cornea to thin and change from a curve into more of a cone shape. Common symptoms include ghosting, multiple images, glare, halos, startbursts around lights and low vision. Often keratoconus can initially be treated with glasses or contact lenses. Once vision can’t be improved with glasses or contact lenses, surgery might be needed.
- Nystagmus is an involuntary repetitive movement of the eyes. It is usually a side to side movement but can be up and down or even a circular motion. People with early onset nystagmus do not usually notice the movement of their vision. Nystagmus is believed to affect approximately 2 in 1000 individuals.
- Retinal Detachment is when the retina peels away from the back of the inside of the eye. It is considered a medical emergency which needs to be treated straight away. One cause of retinal detachment is trauma to the eye. So wear protection for DIY, gardening or any high impact or high speed sports. Regular eye tests are the best way to make sure your eyes are healthy.
- Stargardt Disease is an inherited condition that affects the macular. It is a form of juvenile macular degeneration. It affects around 1 in 10,000 people. The retina is the light sensitive layer on the inner wall of the back of the eye. The macular is the area on the retina which we use for detailed vision such as reading.
- Stroke – Some people have problems with their vision after having a stroke. Visual problems are more common when you suffer a stroke affecting the right side of your brain. The stroke damages the brain and impacts the visual pathways to your eye and cause vision loss, blurry vision, double vision or moving images.
Eye Conditions